Tobacco Cessation Resources
Explore a curated selection of state and national tobacco cessation resources. Click on “View more” on a resource to find more information on what they offer and how to access services.
SELECT A CATEGORY
No description provided
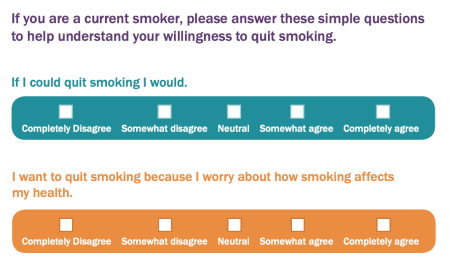
Willingness to Quit Assessment Tool
Are you willing to make a quit attempt?
This short and simple survey helps assess if a patient is willing to make a quit attempt.
When complete, this form can be returned to the healthcare provider.
Created by Pfizer
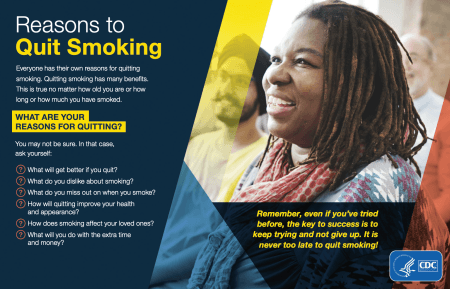
Reasons to Quit Smoking
This visual 1-pager lists some of the many reasons to quit smoking and ways to get help.
Quitting smoking has many benefits. This is true no matter how old you are or how long or how much you have smoked.
Created by the CDC
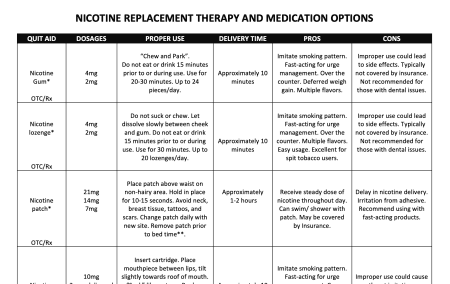
Nicotine Replacement Therapy and Medication Options
A matrix of nicotine replacement therapy and medication options including pros/cons and dosing information.

Tobacco Cessation Change Package
The Tobacco Cessation Change Package was created by the Centers for Disease Control and Prevention (CDC) with the purpose of helping healthcare professionals in outpatient, inpatient, and behavioral health settings, as well as public health professionals who partner with these groups, to implement systems and strategies that improve care for patients who use tobacco.

Tobacco Cessation Guide For Oncology Providers
This guide covers how to talk to patients about tobacco use, motivating patients to stop using tobacco, treating nicotine dependence in patients with cancer, and incorporating tobacco dependence treatment into your practice.
Created by The American Society of Clinical Oncology
Quit Smoking Guide for Patients
Quitting smoking is a great way to improve your health and the health of those around you.
Deciding to quit smoking is the first step toward being a nonsmoker. The information and resources in this guide will help you reach your goal. You will have the best chance of success if you use the guide as a step-by-step workbook.
Five key steps to quit smoking:
- Get ready.
- Get support and encouragement.
- Learn new skills and behaviors.
- Get medicine and use it correctly.
- Be prepared for relapse or difficult situations.
Whether you smoke cigarettes or use other types of tobacco or nicotine products, following these 5 steps will put you on a path to better health. Quitting smoking is hard work. This guide will show you how to quit, but success requires your energy, your determination, and your time. As you begin working toward your goal, keep in mind that half of all people who ever smoked have quit. You can do it, too!
Created by the American Academy of Family Physicians
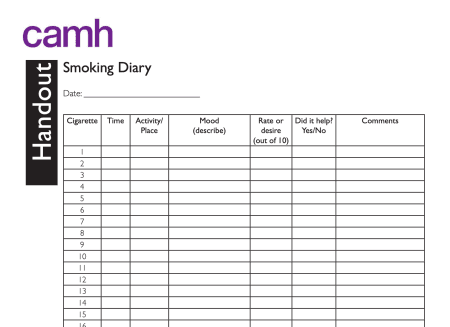
Smoking Diary
A smoking diary 1-page handout to help patients track when they smoke and how it affects their mood. This handout can be used to support a patient's efforts to quit smoking.

Stopping Tobacco Use After a Cancer Diagnosis Patient Toolkit
Resources and Guidance for Patients and Families from the American Society of Clinical Oncology
If you or a loved one has been diagnosed with cancer, quitting tobacco use is one of the best ways to improve the chances of successful cancer treatment. Some people believe that it is too late to quit after a cancer diagnosis, that the damage has already been done. Others believe that the smoking caused their cancer and feel like they have brought this on themselves. People who use tobacco should not blame themselves for a cancer diagnosis or feel that nothing can be done to help them. Quitting can have immediate and long-term benefits.
Created by the American Society of Clinical Oncology
Personalized Quit Plan Template
This clear and simple template helps patients learn about the importance of quitting smoking to improve their health and how to create a quit plan.

Guide to the Nicotine Patch
Why choose the nicotine patch?
- The nicotine patch is used to help you quit smoking by “replacing” the nicotine that you would normally get from a cigarette, but without the harmful chemicals found in cigarette smoke.
- It makes you more comfortable while you are quitting because it reduces the cravings and withdrawal that you feel when you stop smoking.
- It’s easy to use—you apply the patch once a day. Can be used with other nicotine medicines (gum,lozenge, nasal spray, or inhaler)—and studies have shown that this works better than using only the patch when quitting.
- It is inexpensive compared to some of the other medicines for quitting smoking, and is available without a prescription.
Free Continuing Education Courses for Providers
Get access to tools, resources, and educational modules to help you care for your patients with tobacco dependence.
Modules include:
- Best Practices for Tobacco Cessation Using Medication And Behavioral Support
- Michigan Medicaid and Quitline Benefits for Tobacco Cessation
- Special Quitline Programs For Tobacco Cessation
- Connecting The Harms of Tobacco Use to Chronic Health Conditions
- Tobacco Cessation for Behavioral Health Populations
- Vaping and E-Cigarette Devices: What Are They and How Do They Harm?
and more!
*These continuing education modules are offered free of charge by National Jewish Health. *

Pregnancy and Postpartum Tobacco Cessation Program
Quitting tobacco during pregnancy or postpartum is hard, but it’s one of the best ways a woman can protect herself and her baby’s health.
National Jewish Health developed the first tobacco cessation program dedicated to pregnant and postpartum women. For nearly a decade, our Pregnancy and Postpartum Program has given new and expectant moms the support they need to stop using tobacco while they are pregnant and help to prevent relapse after giving birth.
Participants receive:
- Nine telephone coaching sessions (five during pregnancy and four postpartum) with a dedicated female Tobacco
- Cessation Coach. Our Coaches are specially trained to provide coaching during the sensitive physical and emotional times of pregnancy and the postpartum period.
- Nicotine replacement therapies (NRT) with physician consent (if offered by the state).
- A personalized Welcome Packet including special educational materials and the industry renowned My Quit Journey© workbook.
- A suite of eHealth services to supplement telephone coaching including customized email and text messages specific to pregnant and postpartum stages, two-way chat and interactive online resources.
- Incentives for all pregnancy and postpartum completed calls: $10 per completed pregnancy call and $20 per completed postpartum call.
Outcomes from this program have been positive. Women remain engaged in care for longer and a far greater number of women remain tobacco-free after delivery when compared to pregnant women who do not enroll in the program. Call 1-800-QUIT-NOW (1-800-784-8669) or visit Michigan.quitlogix.org.
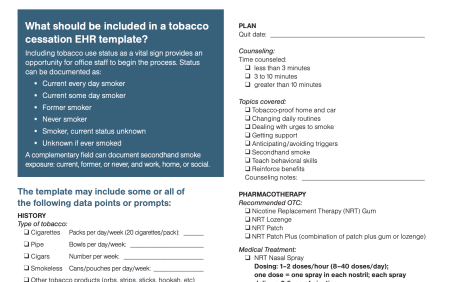
Integrating Tobacco Cessation Into Electronic Health Records
The U.S. Public Health Service Clinical Practice Guideline, Treating Tobacco Use and Dependence, calls for system-level tobacco intervention efforts. Electronic health records (EHRs) allow for integration of this guideline into the practice workflow, facilitating system-level changes to reduce tobacco use.
The American Academy of Family Physicians (AAFP) advocates for EHRs that include a template that prompts clinicians and/or their practice teams to collect information about tobacco and nicotine use, secondhand smoke exposure, cessation interest, and past quit attempts. The EHR should also include automatic prompts that remind clinicians to:
- Encourage quitting
- Advise about smoke-free environments
- Connect patients and families to appropriate cessation resources and materials
The tobacco treatment template should be automated to appear when patients present with complaints such as cough, upper respiratory problems, diabetes, ear infections, hypertension, depression, anxiety, and asthma, and for well-patient exams.
Created by the Academy of Family Physicians

Health Benefits of Quitting Smoking Handout
What are the benefits of quitting smoking?
Many smokers think that because they have smoked for so long the damage has been done and it is too late to quit. This is not true. All smokers, no matter how heavily they smoke, will notice significant benefits after quitting smoking.
Created by the CAMH Knowledge Exchange
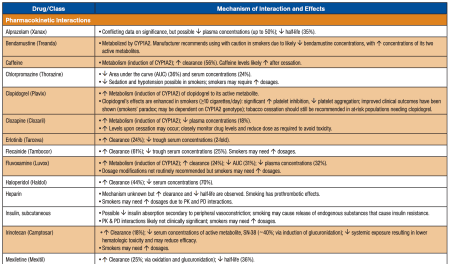
Drug Interactions with Tobacco Smoke
Many interactions between tobacco smoke and medications have been identified. Note that in most cases it is the tobacco smoke—not the nicotine—that causes these drug interactions. Tobacco smoke interacts with medications by influencing the absorption, distribution, metabolism, or elimination of other drugs, potentially causing an altered pharmacologic response. Because of these interactions, smokers may require higher doses of medications. Upon cessation, dose reductions might be needed.
Adapted and updated, from Zevin S, Benowitz NL. Drug interactions with tobacco smoking. Clin Pharmacokinet. 1999;36:425-438. Copyright © 1999-2019 The Regents of the University of California

Implementing Ask, Advise, Refer Guide for Clinicians
Implementation of Ask‐Advise‐Refer is most successful when clinicians and staff work as a team to determine the best method to integrate it into routine patient care.
This helpful guide from RX for Change explains how to implement Ask‐Advise‐Refer in your clinical setting including helpful tips, example dialogue, and additional information.

Tobacco Cessation in the Emergency Department
Tobacco use is the leading preventable cause of death in the United States. Smoking or chewing tobacco may increase a patient’s risk for chronic obstructive pulmonary disease (COPD), coronary artery disease, lung cancer and stroke. While smokers account for less than 14% of the U.S. population, up to 30 to 40% of patients seen in emergency departments are smokers.
With this important knowledge of how many emergency room patients smoke, Yale Medicine is at the forefront of a growing movement to initiate smoking cessation interventions there, including several tobacco intervention-related research studies, says Steven L. Bernstein, MD, an emergency medicine physician and the principal investigator of the Yale Medicine emergency department’s tobacco-related studies.
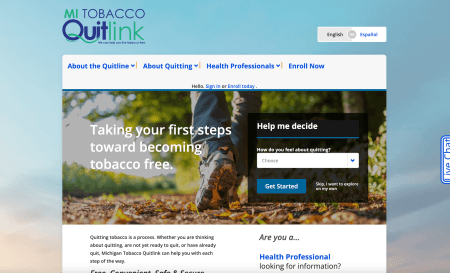
Michigan Tobacco Quitlink
Quitting tobacco is a process. Whether you are thinking about quitting, are not yet ready to quit, or have already quit, Michigan Tobacco Quitlink can help you with each step of the way.
The Quitlink commercial tobacco cessation program uses clinically proven methods to achieve some of the highest quit rates in the country. We help more than 450 people a day in their journey to quit tobacco. With a 37 percent responder quit rate for those who use coaching and nicotine replacement therapy (NRT) and a 90 percent participant satisfaction rate, we are confident in our ability to help your patients live tobacco free.
Tobacco control interventions in the emergency department: a joint statement of emergency medicine organizations
Steven L Bernstein, Edwin D Boudreaux, Rita K Cydulka, Karin V Rhodes, Nadine A Lettman, Sherri-Lynne Almeida, Lynne B McCullough, Selma Mizouni, Arthur L Kellermann, American College of Emergency Physicians Task Force on Smoking Cessation
Smoking is the leading cause of preventable death and illness in the United States. National practice guidelines call for all health care providers to "ask" all patients about tobacco use, and to "advise, assess, assist, arrange" when smokers want to quit smoking (the "5 As").
Emergency departments (EDs) have not been an important locus of tobacco control efforts, although ED patients typically smoke at rates exceeding that of the general population, are interested in quitting, and often have limited access to primary care. To address the role of emergency medicine in tobacco control, the American College of Emergency Physicians convened a task force of representatives of major emergency medicine professional organizations. Funded by the Robert Wood Johnson Foundation, the group met in 2004 and 2005.
This article represents a summary of the task force's recommendations for tobacco control practice, training, and research. We call on emergency care providers to routinely assess patients' smoking status, offer brief advice to quit, and refer patients to the national smokers' Quitline (800-QUIT-NOW) or a locally available program. Given the global burden of tobacco-related illness, the task force considers it essential for emergency physicians to conduct research into the efficacy of ED-based interventions and to place tobacco control into the training curriculum for emergency medicine residencies. Tobacco control fits within the traditions of other ED-based public health practices, such as injury control. ED-based tobacco control would allow the specialty to help fulfill the Healthy People 2010 mandate to reduce the prevalence of smoking among US citizens.

Guide to the Nicotine Inhaler
Why choose the nicotine inhaler?
- The nicotine inhaler is used to help you quit smoking by “replacing” the nicotine that you would normally get from a cigarette, but without the harmful chemicals found in cigarette smoke.
- It makes you more comfortable while you are quitting because it reduces the cravings and withdrawal that you feel when you stop smoking.
- It can satisfy your urges to have something in your hand that you bring to your mouth.
- It can be used with the nicotine patch—and studies have shown that this works better than using only one nicotine replacement medicine.

Guide to Nicotine Gum
Why choose the nicotine gum?
- The nicotine gum is used to help you quit smoking by “replacing” the nicotine that you would normally get from a cigarette, but without the harmful chemicals found in cigarette smoke.
- It makes you more comfortable while you are quitting because it reduces the cravings and withdrawal that you feel when you stop smoking.
- It can be used with the nicotine patch—and studies have shown that this works better than using only one nicotine replacement medicine.
- It is inexpensive compared to some of the other medicines for quitting smoking, and is available without a prescription.

Guide to Nicotine Nasal Spray
Why choose the nicotine nasal spray?
- The nicotine nasal spray is used to help you quit smoking by “replacing” the nicotine that you would normally get from a cigarette, but without the harmful chemicals found in cigarette smoke.
- It makes you more comfortable while you are quitting because it reduces the cravings and withdrawal that you feel when you stop smoking.
- It works more quickly than the nicotine patch, gum, lozenge, and inhaler.
- It can be used with the nicotine patch—and studies have shown that this works better than using only one nicotine replacement medicine.

Guide to Free Or Reduced Cost Smoking Cessation Medication
If you are having a hard time paying for medications that can help you quit smoking, there are programs that may be able to help.
- Medicaid
- Medicare
- Michigan Tobacco Quitline
- The Medicine Assistance Tool
- Pfizer Pathways
Use this guide to help access smoking cessation medications for free or at a reduced cost.

Treating Tobacco Use & Dependence Reference Guide for Clinicians
The Quick Reference Guide for Clinicians contains strategies and recommendations from the Public Health Service-sponsored Clinical Practice Guideline Treating Tobacco Use and Dependence.
The guideline was designed to assist clinicians, smoking cessation specialists, healthcare administrators, insurers, and purchasers in identifying and assessing tobacco users and in delivering effective tobacco dependence interventions. It was based on an exhaustive systematic review and analysis of the extant scientific literature from 1975–2007 and uses the results of more then 50 meta-analyses.

What Happens When Your Patient is Referred to The Michigan Tobacco Quitlink?
This document decribes what happens when a patient is reffered to the Michigan Tobacco Quitlink.

Guide to Nicotine Lozenge
Why choose the nicotine lozenge?
- The nicotine lozenge is used to help you quit smoking by “replacing” the nicotine that you would normally get from a cigarette, but without the harmful chemicals found in cigarette smoke.
- It makes you more comfortable while you are quitting because it reduces the cravings and withdrawal that you feel when you stop smoking.
- It can be used with the nicotine patch—and studies have shown that this works better than using only one nicotine replacement medicine.
- It is inexpensive compared to some of the other medicines for quitting smoking, and it is available without a prescription.
Using a Quitline to Deliver Opt-Out Smoking Cessation for Cancer Patients
Anna E Notier, Polly Hager, Karen S Brown, Laura Petersen, Louise Bedard, Graham W Warren
Although smoking by patients with cancer and survivors causes adverse outcomes, many patients with cancer do not receive access to evidence-based tobacco use treatment. The purpose of this article is to report on delivery of tobacco use treatment to patients with cancer using a state-supported Quitline.
Conclusion: Using statewide resources to increase access to evidence-based smoking cessation assistance to patients with cancer is achievable. In an increasingly cost-conscious health care environment, collaborative initiatives that use or enhance existing resources should be considered and refined to deliver effective evidence-based care.
Uptake and efficacy of using a state quitline to address tobacco use by cancer patients treated in community cancer centers.
Anna E Schulze, Karen Brown, Polly Hager, Laura Petersen, Hilary Baca, Louise Bedard, Graham W. Warren
Smoking by cancer patients and survivors causes adverse outcomes. Cancer treatment guidelines recommend evidence-based cessation support for all patients who use tobacco. However, there is little information on using existing state quitlines to provide support for cancer patients during and following cancer treatment.
Conclusion: Partnering community oncology practices with quitlines can significantly increase access and delivery of evidence-based support. Results support integration of existing cessation resources into oncology practice to facilitate broad uptake.

Freedom From Smoking® at Henry Ford Health
Freedom From Smoking® is a group quitting class facilitated by one of Henry Ford's trained tobacco treatment experts.
Freedom From Smoking classes provide group treatment for tobacco dependence and consist of 8 sessions over the course of 7 weeks. The group prepares for a shared "quit day" by learning about medications that can help them stop, lifestyle changes that make quitting easier, and how to stay smoke-free for good. As the weeks continue you will receive structured support and advice from fellow group members and staff.
Freedom From Smoking
Website and other resources designed by the American Lung Association to help people quit smoking. Freedom From Smoking has been helping people quit smoking for 35 years and has been ranked as one of the most effective cessation programs in the country.
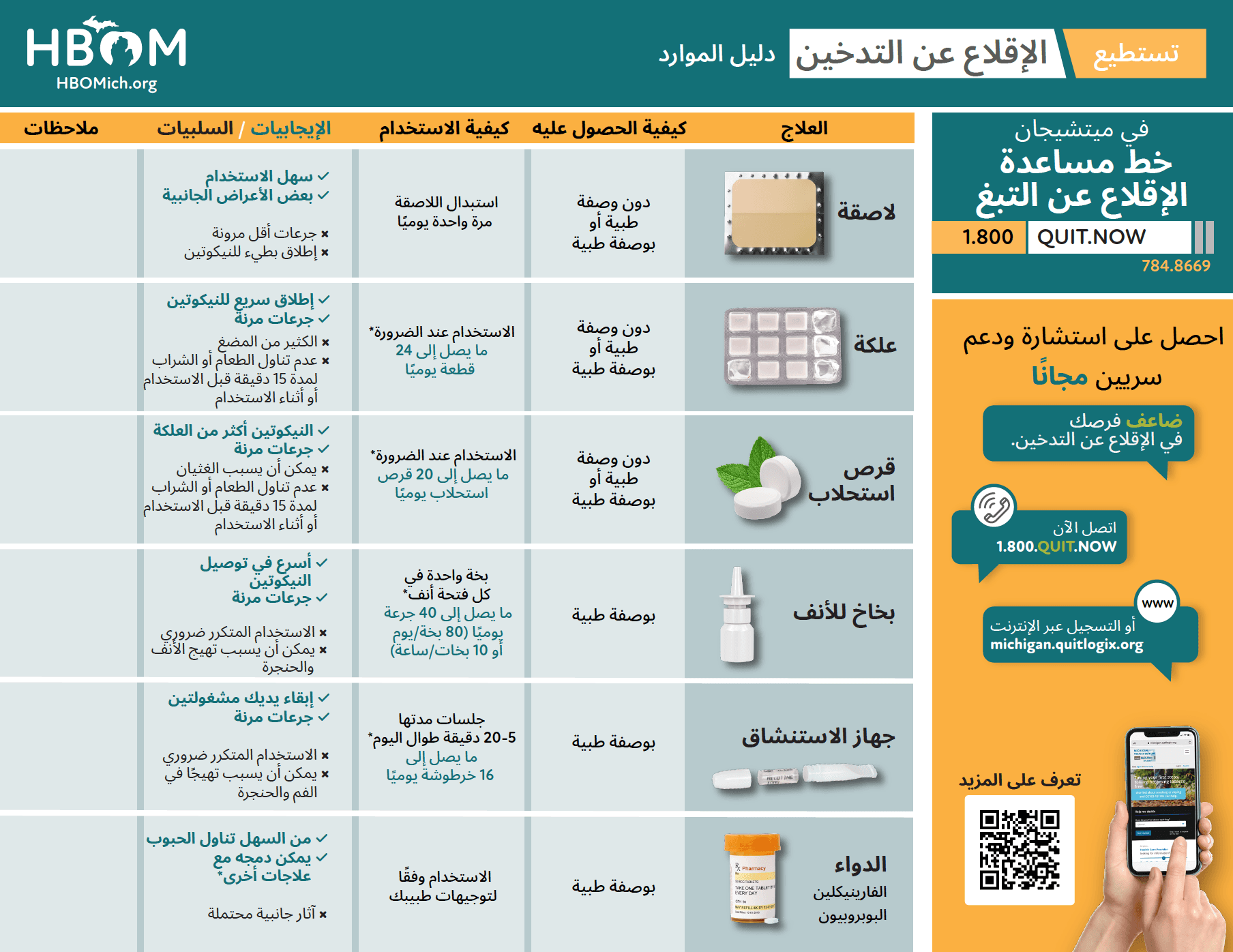
HBOM Nicotine Replacement Therapy Guide (Arabic)
يقدم هذا الدليل المرئي نظرة عامة عالية المستوى على العلاج ببدائل النيكوتين وكيفية استخدامه. يتضمن الدليل أيضًا روابط ورمز QR إلى Michigan Tobacco Quitline.
Help Your Patients Quit Tobacco Use
Tobacco use and dependence is a chronic, relapsing condition that, like other chronic diseases, may require repeated intervention and long-term support. Most people who use tobacco want to quit, but most try to quit multiple times before succeeding. As a healthcare professional, you play a critical role in helping people quit using tobacco.
Clinical Intervention Works
- Even brief advice from a provider increases the chance a patient will try to quit.
- Counseling and medication can double a patient’s chances of quitting.
- Providing tobacco dependence treatment is reimbursable and covered as a preventive service.
- Providing tobacco cessation support increases patient satisfaction with care.
Created by the CDC
A Practical Guide to Help Your Patients Quit Using Tobacco
This guide provides simple steps and suggested language that you can use to briefly (3 to 5 minutes) intervene with patients who use tobacco. These steps can be integrated into the routine clinical workflow and can be delivered by the entire clinical care team.
Key considerations for treating tobacco dependence:
- Behavioral counseling can benefit all patients
- Medication can help patients quit and can be used with most patients, though special considerations may apply for some individuals.
- Combining behavioral counseling and medication is more effective than either treatment alone.
- Follow-up is key to monitoring patients for treatment adherence, side effects, and efficacy, along with providing support and continued assistance.
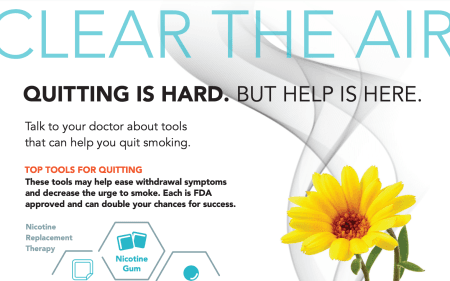
Clear the Air: Quitting is Hard Infographic
1-page visual handout with top tools for quitting.
*Created by the AAFP *
IT'S TIME: Helper's Guide
A First Nations-specific toolkit for commercial tobacco cessation.
The purpose of this toolkit is to support helpers in offering commercial tobacco interventions with First Nations. It is organized into six circles with each circle focusing on specific learning outcomes.
The goal of the circles will be to support First Nations in:
- Preparing for their commercial tobacco cessation or reduction journey (e.g., thinking about quitting or reducing).
- Mapping their commercial tobacco cessation or reduction journey (e.g., developing a plan to quit or reduce).
- Staying with their commercial tobacco cessation or reduction journey (e.g., learning ways to prevent resuming smoking)
IT’S TIME: First Nations Quit Toolkit
A First Nations-specific toolkit for commercial tobacco cessation.
Indigenous Tools and Strategies on Tobacco including interventions, medicines and education.

Withdrawal Symptoms Information Sheet
Quitting tobacco use brings about a variety of physical and psychological withdrawal symptoms. For some people, coping with withdrawal symptoms is like riding a roller coaster—there can be sharp turns, slow climbs, and unexpected plunges. This sheet covers common symptoms of tobacco withdrawl and how to cope with them.
Created by Rx for Change
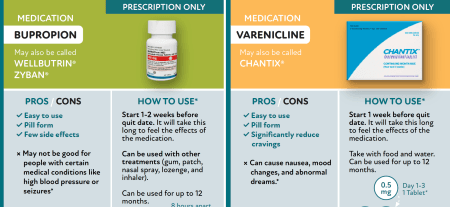
HBOM Tobacco Cessation Medications Card
This visual card is designed to be printed as a postcard and shows the two medication options for tobacco cessation including pros/cons and dosing information. On the back, it provides information on the Michigan Tobacco Quitline and how to contact them.
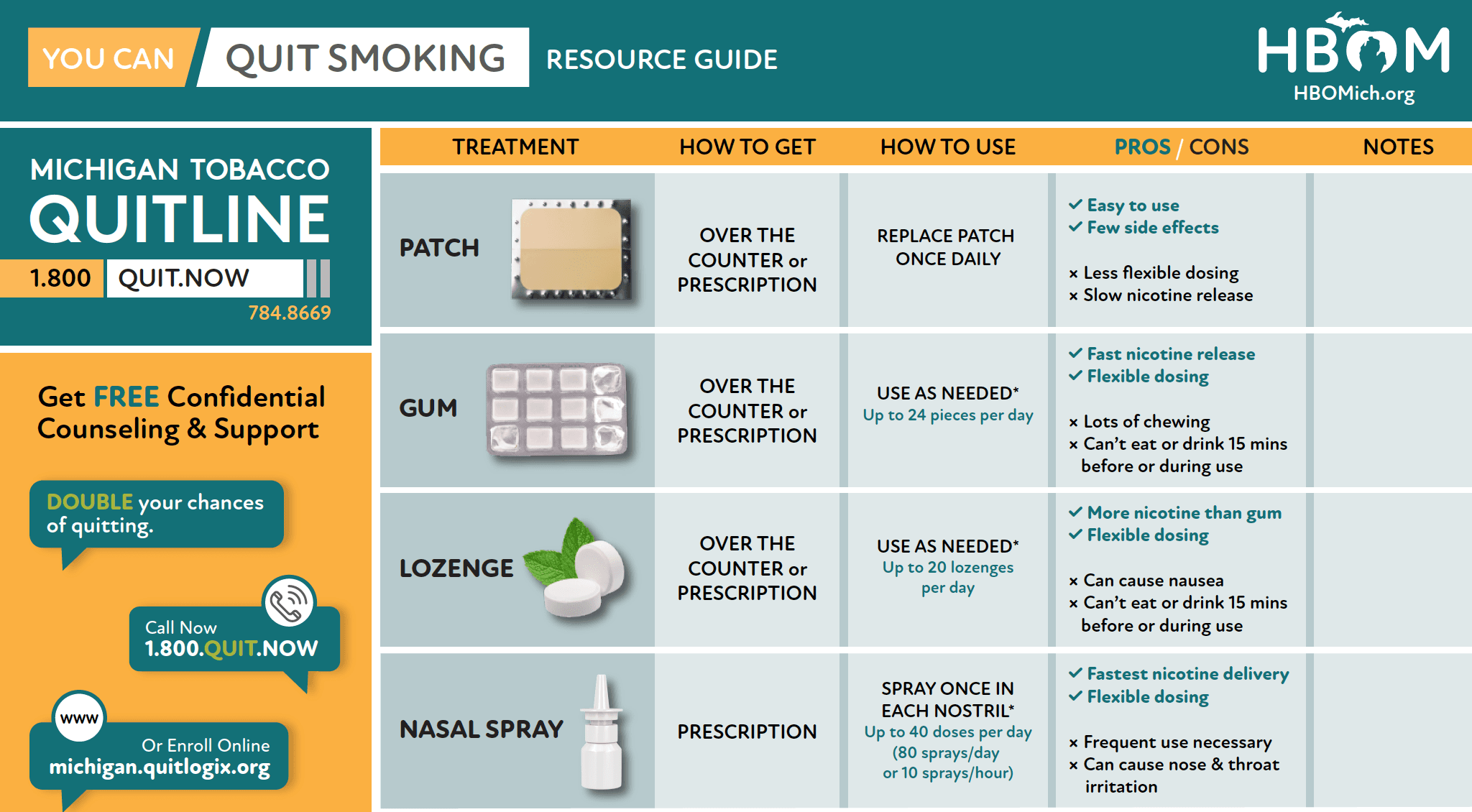
HBOM Nicotine Replacement Therapy Guide
This visual guide provides a high-level overview of nictotine replacement therapy and how to use them. The guide also includes links and a QR code to the Michigan Tobacco Quitline.

Pregnant and Smoking MDHHS Flyer
This easily printable 1-page flyer encourages pregnant women to quit smoking and call the Michigan Tobacco Quitline for support.
Did you know?
- Smoking can cause you to deliver too soon.
- By quitting, you're making sure your baby is getting enough oxygen to grow.

Make Your Own Cinnamon Toothpicks
Toothpicks can be a great tool when quitting tobacco. They can keep your hands and mouth busy during cravings and many quitters like the distraction that intense flavors like cinnamon or mint can give.
Use these simple instructions to make your own flavored toothpicks.

Choosing a Health Insurance Plan: Tobacco Users
This guide provides questions and answers tobacco users who want to quit should consider when selecting a health insurance plan.
Q: I’m a smoker, but I eventually want to quit. What should I think about when choosing a health insurance plan?
A: There are several things for current and potential “quitters” to consider when choosing a health insurance plan...
Created by the American Lung Association

Myths about Tobacco Use
A list of myths and facts about tobacco use. For example:
Myth: Tobacco is not a drug.
Fact: The nicotine found in tobacco products is a very addictive drug. Addiction to nicotine has been compared to having an addiction to drugs like cocaine or heroin. Exposure to nicotine alters brain chemistry resulting in tobacco dependence and nicotine addiction.
Created by the MHealthy Tobacco Consultation Service

Helpful Tips To Make Quitting Easier
This helpful 1-pager provides a list of a tips, coping strategies, and benefits of quitting smoking. This can be used as a high level overview of information when talking to patients about quitting.
*This resources was created by Mhealthy Tobacco Consultation Service and encourages patients to contact their services. If you are outside of the University of Michigan system, consider copying the information to an appropriate format for your health system. *
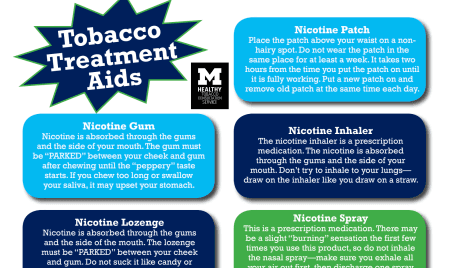
Tobacco Treatment Aids
A visual guide for tobacco treatment aids including nictotine replacement therapy and medications.
Created by MHealthy Tobacco Consultaton Service

Things to do other than using tobacco
A helpful list of things you can do when you're having a craving or are experiencing nicotine withdrawal symptoms.
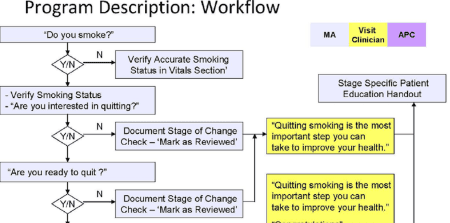
Harvard Vanguard Work Flow For Interventions With Smokers
An example clinical work flow for tobacco cessation interventions.
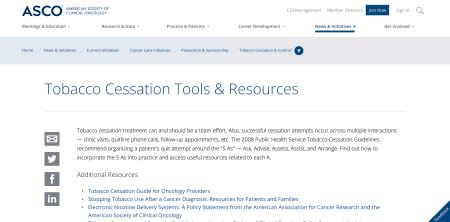
Tobacco Cessation Tools & Resources from the American Society of Clinical Oncology
Tobacco cessation treatment can and should be a team effort. Also, successful cessation attempts occur across multiple interactions — clinic visits, quitline phone calls, follow-up appointments, etc.
The 2008 Public Health Service Tobacco Cessation Guidelines recommend organizing a patient's quit attempt around the "5 As" — Ask, Advise, Assess, Assist, and Arrange. Find out how to incorporate the 5 As into practice and access useful resources related to each A.
Assessing Tobacco Use by Cancer Patients and Facilitating Cessation: An American Association for Cancer Research Policy Statement
Benjamin A. Toll, Thomas H. Brandon, Ellen R. Gritz, Graham W. Warren, Roy S. Herbst, and Writing Committee for the AACR Subcommittee on Tobacco and Cancer
When diagnosed with cancer, patients can immediately make a meaningful positive impact on their health by stopping their tobacco use. Scientific evidence clearly shows that tobacco use in patients with cancer leads to poorer outcomes. The specific biological processes driving tobacco consumption’s interference in cancer therapy are the subject of continuing research, but the evidence is clear that tobacco use in patients with cancer leads to decreased treatment efficacy and safety, decreased survival, decreased quality of life, increased treatment-related toxicity, and increased risk of cancer recurrence and second primary tumors. Data suggest that tobacco cessation can improve outcomes and survival in patients with cancer, yet full execution of evidence-based cessation interventions is infrequent in oncology settings. Therefore, both improved provision of cessation assistance to all patients with cancer who use tobacco or have recently quit and further study of the deleterious effects of tobacco use and benefits of tobacco cessation on cancer progression and treatment are needed and recommended by the American Association for Cancer Research. Progress on both fronts begins with universal assessment and documentation of tobacco use as a standard of quality cancer care regardless of treatment setting and will be further facilitated through the development of reliable, valid, and standard measures of tobacco use, incorporation of evidence-based procedures into quality and accreditation procedures, and the development of appropriate training, clinical infrastructure, and incentives for delivery of tobacco cessation interventions.
Smoking at diagnosis and survival in cancer patients
Graham W. Warren, Karin A. Kasza,Mary E. Reid, K. Michael Cummings, James R. Marshall
The effect of smoking on survival in cancer patients is limited by the lack of structured prospective assessments of smoking at diagnosis. To assess the effect of smoking at diagnosis on survival, structured smoking assessments were obtained in a cohort of 5,185 cancer patients within 30 days of a cancer diagnosis between 1982 and 1998. Hazard ratios (HRs) or odds ratios were generated to analyze the effects of smoking at diagnosis on overall mortality (OM) and disease-specific mortality (DSM) in a patient cohort from 13 disease sites containing at least 100 patients in each disease site. With a minimum of 12 years of follow-up, current smoking increased OM risk versus recent quit (HR 1.17), former (HR 1.29) and never smokers (HR 1.38) in the overall cohort. Current smoking increased DSM risk versus former (HR 1.23) and never smokers (HR 1.18). In disease sites with proportionately large (>20%) recent quit cohorts (lung and head/neck), current smoking increased OM and DSM risks as compared with recent quit. Current smoking increased mortality risks in lung, head/neck, prostate and leukemia in men and breast, ovary, uterus and melanoma in women. Current smoking was not associated with any survival benefit in any disease site. Data using prospective structured smoking assessments demonstrate that current smoking increased long-term OM and DSM. Standardized smoking assessment at diagnosis is an important variable for evaluating outcomes in cancer patients.

FAQs for Helping Someone Quit (Smokefree.gov)
How much support should I give someone quitting smoking? Everyone who quits needs a different amount or type of support. Just ask them what kind of support they want and how much.

Relapsed Smokers Who Are Ready To Try Again: What To Do?
A 3-STEP PROTOCOL FOR CLINICIANS
Many individuals who relapse back to smoking do so because they fail to plan. Often, patients think that they can simply “make” themselves quit and do not avail themselves of the many proven behavior change programs provided by various sources. Furthermore, most smokers do not use a cessation medication or, if they do, they use it incorrectly. Generally speaking, patients significantly under-dose or stop pharmacologic therapy too soon.
You can help patients who relapse regain abstinence by encouraging them to learn from their prior experiences rather than use those experiences as proof that they cannot quit. To underscore this perspective, advise patients that the best way to quit smoking is to combine a behavior change program with a cessation medication. The following 3-step protocol will help you provide this information in an efficient, effective manner for patients who are ready to try again.

Tobacco Cessation Counseling Guidesheet
A guide for using the 5As with patients including suggested dialogue for each step.
Step One: ASK about Tobacco use Step Two: ADVISE to Quit Step Three: ASSESS Readiness to Quit Step Four: ASSIST with Quitting Step Five: ARRANGE Follow-up Counseling

Coping With Quitting: Cognitive And Behavioral Strategies
COGNITIVE STRATEGIES focus on retraining the way a patient thinks. Often, patients will deliberate on the fact that they are thinking about a cigarette, and this leads to relapse. Patients must recognize that thinking about a cigarette doesn’t mean they need to have one
BEHAVIORAL STRATEGIES involve specific actions to reduce risk for relapse. These strategies should be considered prior to quitting, after determining patient-specific triggers and routines or situations associated with tobacco use. Below are strategies for several of the more common cues or causes for relapse.

Guide to Bupropion
A simple guide to using Bupropion for tobacco cessation.
Information includes: Why choose bupropion SR? How do I use bupropion SR? Dosing schedule How long is the treatment? What are the side effects of bupropion SR? What else do I need to know?

Guide To Free Or Reduced Cost Smoking Cessation Medication
If you are having a hard time paying for medications that can help you quit smoking, there are programs that may be able to help.
This guide includes instructions for accessing cost assistance programs through Medicaid, Medicare, the Michigan Tobacco Quitline, The Medicine Assistance Tool, and Pfizer.
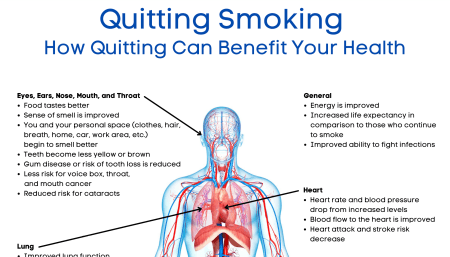
Quitting Smoking: How Quitting Can Benefit Your Health
A visual 1-pager listing the ways that quitting smoking can benefit different parts of your body.

Planning For Change: Thinking About Quitting Patient Worksheet
This simple worksheet helps patients plan to quit smoking and reflect on their motivations and previous attempts.
Understanding the reasons why you smoke, in addition to considering your smoking patterns and routines, are important to the design of a successful quitting plan. Consider the following before you quit:
- Why do I still smoke?
- Why is quitting important?
- What were your main difficulties with quitting in the past?
- What are your barriers to quitting now?
- Are you ready to quit now?
Smokers don’t plan to fail. Most fail to plan. To plan for quitting, you should:
(1) identify triggers for smoking and how to cope with them, (2) identify persons to help you throughout your quit attempt, and (3) choose the best methods—for you—for quitting
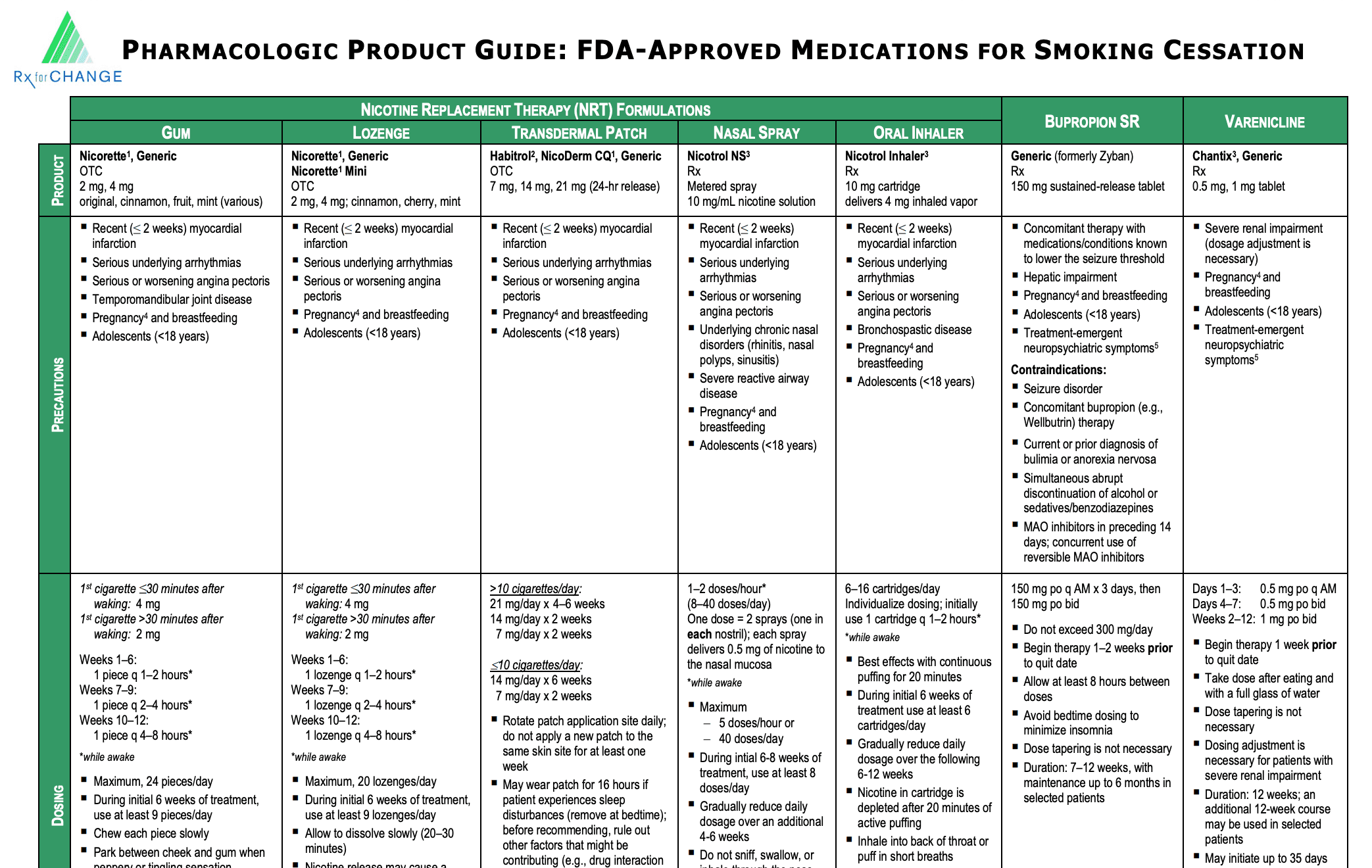
Pharmacologic Product Guide: FDA-Approved Medications for Smoking Cessation
Table detailing dosing, cost, adverse effects, etc for all nictoine replacement therapy and cessation medication options created by RX For Change.
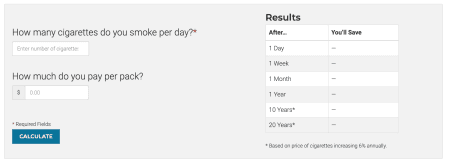
Quit Calculator
How much will you save if you quit smoking?
Smoking cigarettes is expensive. Use this calculator to find out how much of your money is going up in smoke.
CDC: The Benefits of Quitting Smoking
"Quitting smoking has health benefits at any age, no matter how long or how much you have smoked."
Quitting smoking is one of the most important actions people can take to improve their health. This is true regardless of their age or how long they have been smoking.
Quitting smoking:
- reduces the risk of premature death and can add as much as 10 years to life expectancy.
- improves health status and enhances quality of life.
- reduces the risk for many adverse health effects, including poor reproductive health outcomes, cardiovascular diseases, chronic obstructive pulmonary disease (COPD), and cancer.
- benefits people already diagnosed with coronary heart disease or COPD. benefits the health of pregnant women and their fetuses and babies.
- reduces the financial burden that smoking places on people who smoke, healthcare systems, and society.
CDC Quit Smoking Tips
Highlights the stories of people living with chronic conditions related to smoking or secondhand smoke + the effect on family members; focuses on multiple health issues created or exacerbated by smoking; many tools available for both smokers and healthcare providers/pharmacists; info on quit-smoking medicines
Text "CDC" to 47848 to access text support.

My Life My Quit
Free and confidential service for teens who want help quitting all forms of tobacco (including vaping).
Text "start my quit" to 36072 to join.

Varenicline Also known as Chantix® (no generic available)
Why choose varenicline?
- Varenicline is used to help you quit smoking.
- It makes you more comfortable while you are quitting because it reduces the cravings and withdrawal that you feel when you stop smoking.
- Research studies show that varenicline is the most effective medicine for quitting smoking.

“Why do I smoke?”quiz
If you know the answer to this question, it will be easier to stop smoking because you can find ways to make up for the things you may miss when you stop. Most people smoke for different reasons at different times. Reasons for smoking include psychological issues, habits, social pressures and physical dependence on nicotine. The questionnaire that follows will help you decide which reasons are important in your smoking.
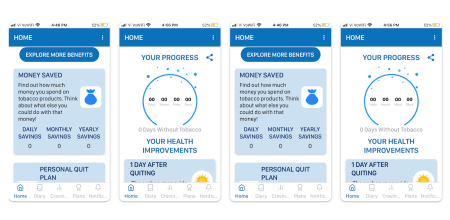
Kwit App
Inspired by Cognitive and Behavioral Therapy (CBT), Kwit helps you to achieve a smoke-free life. It offers you solutions to cope with cravings to smoke and vape.
Track your progress day by day and see how far you've come thanks to the stop smoking counters. The application counts for you the days spent without cigarettes, the money saved, the cigarettes not smoked and many other things.
This stop smoking application is free to download and ad-free. It includes:
- Getting help to stop smoking
- Reducing your consumption of nicotine substitutes
- Stopping vaping
- Keeping track of your consumption of gums and/or patches
- Overcoming your cravings
- Keeping track of your smoking cessation
- Understanding your cravings and emotions
- Finding new ways to quit smoking
Free with in-app purchases including a premium subscription option

Smoke Free - Quit Smoking Now App
This is the app takes a science-based approach to quitting smoking. Over 40 different, evidence-based, techniques will help you get - and stay - smoke free. See and celebrate how long you’ve been quit, how your health is improving how much money you're saving, how many cigarettes you've not smoked, how much life you've regained, and more.
Get tips on dealing with cravings, add notes to see what patterns can be identified and use the graph to see how they're decreasing. Save up for treats to buy yourself with the money saved from not smoking, and remind yourself why it is so important that you stay strong.
Free with in-app purchases

Quit Smoking Virtual Support Group at Henry Ford Health
It’s hard to quit smoking when you are doing it alone. Your chances of success greatly improve when you have a good support system. The Henry Ford Quit Smoking Support Group makes giving up tobacco and vaping easier by providing the support needed to overcome the physical, emotional, and behavioral dependence on tobacco. Get tips and tricks and talk with people going through the same thing in a safe and encouraging space.
The support group is run by Aimee Richardson, Henry Ford Tobacco Treatment Counselor and Certified Health Coach.
The virtual support group meets every Thursday at noon and you can join at any time.
A Perioperative Smoking Cessation Intervention with Varenicline: A Double-blind, Randomized, Placebo-controlled Trial
Jean Wong, M.D., F.R.C.P.C.; Amir Abrishami, M.D.; Yiliang Yang, M.D.; Amna Zaki, M.B.B.S.; Zeev Friedman, M.D., F.R.C.P.C.; Peter Selby, M.B.B.S., C.C.F.P., F.C.F.P.; Kenneth R. Chapman, M.D., M.Sc., F.R.C.P.C.; Frances Chung, M.B.B.S., F.R.C.P.C.
The efficacy of perioperative tobacco interventions on long-term abstinence and the safety of smoking cessation less than 4 weeks before surgery is unclear. Our objective was to determine the efficacy and safety of a perioperative smoking cessation intervention with varenicline to reduce smoking in elective surgical patients.
A perioperative smoking cessation intervention with varenicline increased abstinence from smoking 3, 6, and 12 months after elective noncardiac surgery with no increase in serious adverse events.
Research And Resources on Tobacco
Powered by Truth Initiative Schroeder Institute®
Get the latest facts and analyses on the most important issues in tobacco and substance use.
WHO QuitTobacco App
This WHO QuitTobacco app has been developed based on scientifically proven and WHO advocated methods and strategies to help tobacco users successfully quit use of tobacco. The app can be used by both smokers and users of smokeless tobacco products.
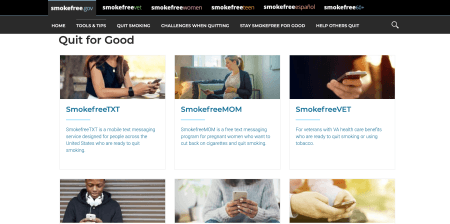
Smokefree Text Programs
Smokefree.gov offers free text messaging programs that give 24/7 encouragement, advice, and tips for becoming smokefree and being healthier. Find the program that meets your needs. You can sign up or opt-out at any time.
Text programs include:
- SmokefreeTXT (English and Spanish options)
- SmokefreeMOM
- SmokefreeVET (English and Spanish options)
- Daily Challenges
- Practice Quit

quitSTART App
The quitSTART app is a free smartphone app that helps you quit smoking with tailored tips, inspiration, and challenges.
The quitSTART app helps you:
- Get ready to quit with tips and information to prepare you for becoming smokefree
- Monitor your progress and earn badges for smokefree milestones and other achievements
- Get back on track if you slip and smoke
- Manage cravings and bad moods in healthy ways
- Distract yourself from cravings with games and challenges
- Store helpful tips, inspirations, and challenges in your Quit Kit
- Share your progress and favorite tips through social media

QuitGuide App
QuitGuide is a free app that helps you understand your smoking patterns and build the skills needed to become and stay smokefree. Use the app to track your cravings by time of day and location, and get motivational messages for each craving you track.
QuitGuide helps you:
- Track cravings and slips by times of day and location
- Track your mood and smoking triggers
- Stay motivated with inspirational messages
- Identify your reasons for quitting
- Get tips and distractions for dealing with cravings and bad moods
- Monitor your progress toward achieving smokefree milestones
- Create journal entries
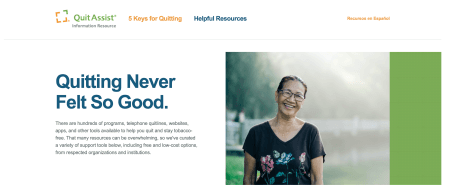
Quit Assist Information Resource
Quitting Never Felt So Good.
There are hundreds of programs, telephone quitlines, websites, apps, and other tools available to help you quit and stay tobacco-free. That many resources can be overwhelming, so we've curated a variety of support tools below, including free and low-cost options, from respected organizations and institutions.
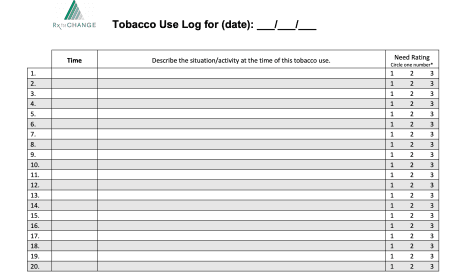
Tobacco Use Log
The Tobacco Use Log can help patients to identify activities or situations that trigger the desire to smoke or use other forms of tobacco. It is important for patients to understand these environmental cues so that they can develop coping strategies to overcome the temptation to use tobacco.
Clinicians can use this information to suggest alternative behaviors to increase the likelihood of a successful quit attempt. The log is most appropriate for patients who are preparing for a quit attempt, but it can be used with any patient who wants to learn more about his or her smoking behavior.
Instructions for use: The Tobacco Use Log is a piece of paper that is kept with the patient’s tobacco. It can be folded and wrapped around the cigarette pack or can of snuff with a rubber band. Alternatively, patients may keep the log in their wallet or day planner. It is important that the log be readily available at the times when the patient uses the tobacco. Through careful documentation of tobacco use over a period of several days, patient-specific tobacco usage patterns become evident.

CDC Tips from Formers Smokers: Reasons to Quit Smoking Patient Handbook
Quitting smoking has many benefits. This is true no matter how old you are or how long or how much you have smoked. This patient booklet includes reasons to quit smoking from actual former smokers. These include:
- Health & Appearance Reasons
- Lifestyle Reasons
- Family & Loved Ones Reasons
It is also includes contact information for the national tobacco QuitLine and links to eductional information on the CDC webpages.
Rx For Change: Clinician-Assisted Tobacco Cessation
Clinician-Assisted Tobacco Cessation is a comprehensive tobacco cessation training program that equips health professional students and practicing clinicians, of all disciplines, with evidence-based knowledge and skills for assisting patients with quitting. Our program draws heavily from the U.S. Public Health Service Clinical Practice Guideline for Treating Tobacco Use and Dependence, in that it advocates delivery of tailored behavioral counseling interventions in conjunction with pharmacotherapy. We address all forms of tobacco, not just cigarettes, and our materials focus on counseling all patients—regardless of their readiness to quit. All materials have undergone extensive external review by key experts in the field.
WebMD Tobacco Coaching
Tools, resources, and support to help you quit smoking.
Spectrum Health Quit Classes
Spectrum Health cessation classes are free, 4-week sessions. Classes are led by a certified tobacco treatment specialist and former smoker over Microsoft Teams.
University of Michigan Tobacco Consultation Service
Available for University of Michigan students, faculty/staff and their spouses/eligible adults, as well as Michigan Medicine patients.

Blue Cross Complete of Michigan: Tobacco Quit Program
The program offers:
- Help creating a plan to quit smoking or chewing tobacco
- Guidance, support and encouragement to stick with your plan to quit – Group and individual counseling or coaching
- Medicines to help you quit
- Blue Cross Complete of Michigan covers all of the over-the-counter and prescription medicines that may be used to help you quit using tobacco. These medicines are covered at your pharmacy with a prescription from your doctor. Over-the-counter medicines may include generic forms of these products, such as Nicorette® (gum or patch) and Commit® (lozenge).
- Prescription medicines may include Chantix®, Nicotrol® inhaler, cartridges and nasal spray, generic Zyban® (bupropion) and others.
How to enroll:
To enroll in the Tobacco Quit Program, call 1-800-QUIT-NOW (784-8669), 24 hours a day, seven days a week. TTY users should call 1-888-229-2182.
DIMENSIONS
DIMENSIONS is a free 16-week tobacco cessation group that provides adults who want to quit smoking with the tools and support to achieve their goals.
The group will meet to cover topics such as stress management, wellness, and behavior change techniques. Classes meet online or in-person based on your individual preference.
The program is free and open to the public. Offered by West Michigan Community Mental Health.
BecomeAnEX
BecomeAnEx offers a diversity of free and well-designed online tools and support for tobacco cessation. Developed in partnership with Mayo Clinic.

Asian Smokers Quitline
Participants receive tobacco cessation counseling with language and cultural background in mind.
Phone counselors are available 10a.m-12a.m EST, M-F. 1-800-838-8917 (Chinese), 1-800-556-5564 (Korean), 1-800-778-8440 (Vietnamese)
American Indian Commercial Tobacco Program
Culturally sensitive phone counseling focused on commercial tobacco use (does not discourage the use of ceremonial tobacco) and recognizes the sacredness of the medicine wheel for Native populations.
McLaren Michigan Freshstart Tobacco Cessation program
Practical counseling and problem-solving skills, education about medication; program offerings for different McLaren areas (Northern MI, Bay Region, Macomb).
This program is designed to help participants stop smoking by providing essential information, skills for coping with cravings, and group support.
cost: $25
Munson Healthcare Freedom From Smoking
Uses the American Lung Association's Freedom From Smoking Program (8 group sessions) offered 3x per year. Individual phone counseling options are also offered.

Henry Ford Freedom From Smoking
Uses the American Lung Association's Freedom From Smoking Program (8 group sessions). Henry Ford offers a special discount on acupuncture to support quitting tobacco for those enrolled in the Tobacco Treatment Service.
Smokefree.gov
Offers a text program for diverse audiences along with 24/7 online support. This is a great resource for those who want to attempt quitting with online or phone assistance.
Text 'QUIT' to 47848 to access text support.